
Every year, diseases of the musculoskeletal system worry more and more people, and their development at an early age is increasingly observed. This is facilitated not only by a change in lifestyle, but also by an increase in the level of injuries, which is largely interconnected. One of the most common pathologies of the musculoskeletal system is osteoarthritis of the hip joint, which is characterized by the appearance of progressive pain and limitation of mobility. Ultimately, the disease can lead to complete joint immobility and disability. In order to avoid the occurrence of such undesirable consequences, it is important to start treatment of arthrosis as soon as possible. And if in the early stages of development it can be stopped with conservative methods, then in case of severe changes it is possible to restore the functions of the hip joint and eliminate excruciating pain only with the help of a high-tech operation.
What is osteoarthritis of the hip joint?
Osteoarthritis of the hip joint is a chronic degenerative-dystrophic disease in which progressive destruction of the hip joint occurs. At the same time, all its components gradually become involved in the pathological process, but hyaline cartilage is especially affected, which leads to a narrowing of the joint space and deformation of its other components. Most often, the pathological changes occur in only one hip joint, although both can also be affected simultaneously.
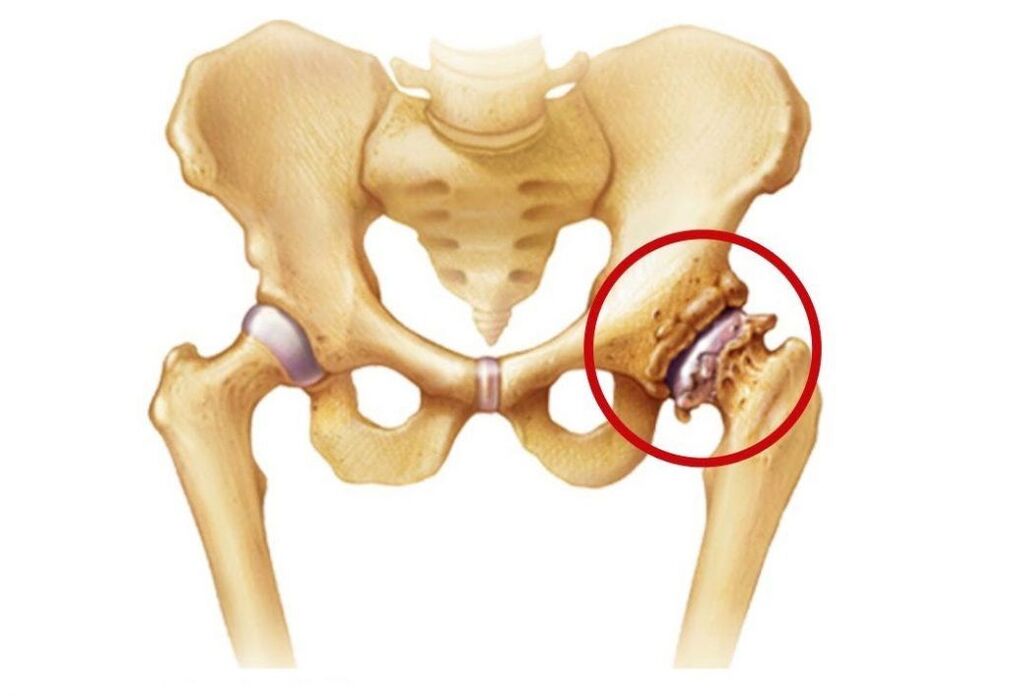
The hip joints are the largest in the human body, bearing the greatest load during the day. Each of these is made up of the head of the femur and the acetabulum, which is a bowl-shaped depression in the pelvis. Both surfaces are covered with smooth, moderately elastic hyaline cartilage. It is he who ensures the smoothness and unimpeded sliding of the femoral head in a natural depression, and thus allows movements in several planes.
Movement of the hip joint is provided by a group of muscles connected to it by fasciae. It is also surrounded by ligaments, the tasks of which are to limit its mobility within physiological limits and ensure the stability of its position.
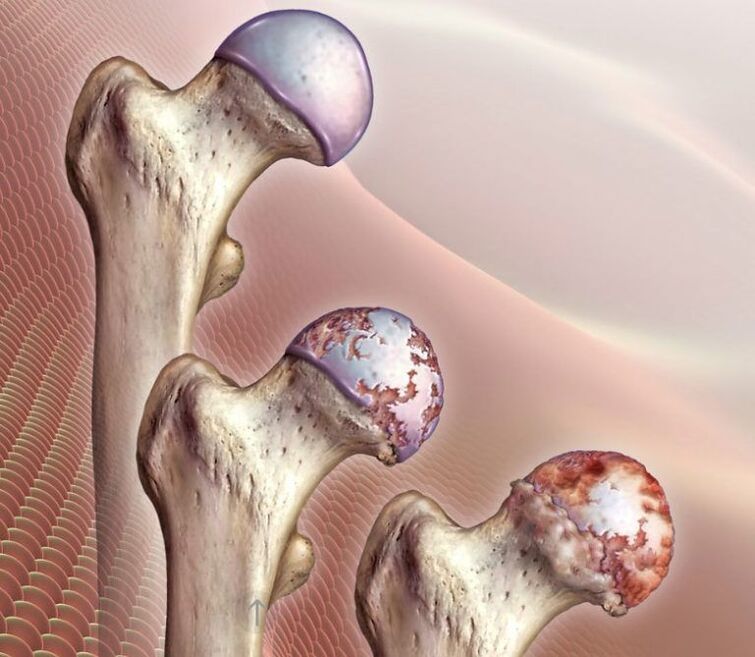
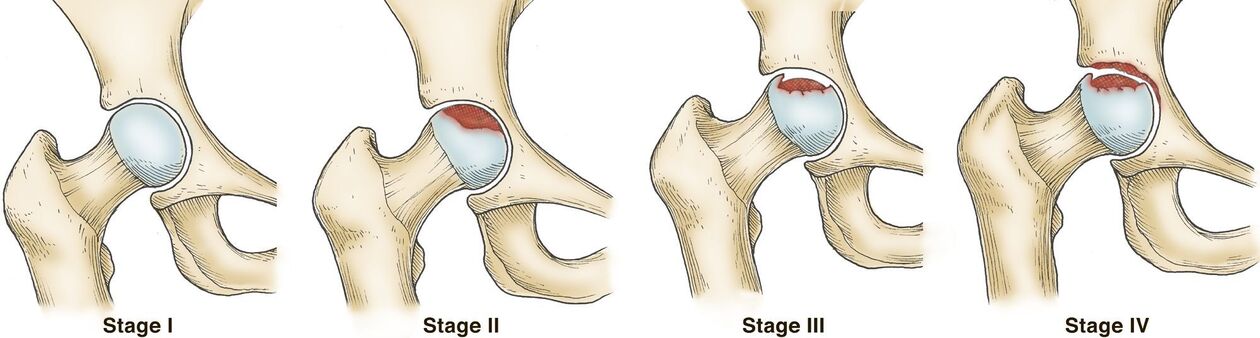
The entire joint is surrounded by a joint capsule covered by a synovial membrane. Its main task is the synthesis of synovial fluid, which lubricates the adjoining parts of the hip joint and at the same time acts as a carrier of nutrients for it. It is from the synovial fluid that the hyaline cartilage that lines the femoral head and the surface of the acetabulum constantly receives components for the formation of new cells, that is, regeneration. This is extremely important for this cartilaginous formation, since with each movement of the hip it wears out, but normally it is replaced immediately. But when injured or under the influence of other factors, this does not happen, which leads to the development of arthrosis of the hip joint, that is, thinning and destruction of its hyaline cartilage.
As a result, deformed areas are formed on ideally smooth cartilage, which increase as the pathology progresses. As it wears, the surfaces of the bones that form the joint are exposed. When they come into contact, there is a characteristic cracking sound and severe pain. This causes osteophytes to form and, in the final stages of development, the femoral head fuses completely with the acetabulum, making any movement in the hip joint impossible.
At the same time, arthrosis of the hip joint can provoke the development of various inflammatory processes within the joint, including:
- bursitis - inflammation of the synovial bag;
- tendovaginitis - an inflammatory process in the sheath of the sheath of the tendons of the muscles;
- tunnel syndrome - compression of the nerves, causing radiating pain along the strangulated nerve.
The reasons
One of the common causes of the development of arthrosis of the hip joint is mechanical damage, not only direct injuries, but also microdamage caused by the destructive effect of excessive loads on it. One of the most common causes of the development of the disease is a fracture of the femoral neck.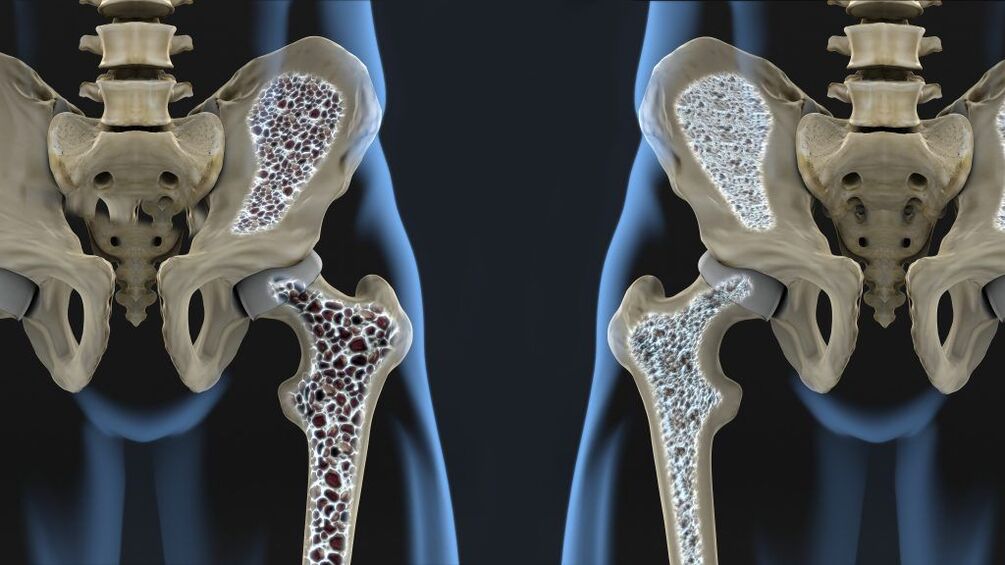 It exits the femur at an angle of 120° and connects it to the head. The presence of osteoporosis significantly increases the probability of suffering a hip fracture, but this type of injury can also be the result of a traffic accident, fall from a height, impact, etc.
It exits the femur at an angle of 120° and connects it to the head. The presence of osteoporosis significantly increases the probability of suffering a hip fracture, but this type of injury can also be the result of a traffic accident, fall from a height, impact, etc.
A fracture of the femoral neck may be accompanied by aseptic necrosis of the femoral head, which will become a trigger for the development of degenerative-dystrophic changes in the joint. The presence of dysplasia or subluxation of the hip joint, ruptures of its ligaments, transcondylar fractures or fractures of the acetabulum also create favorable conditions for the damage of its structures. In such situations, post-traumatic arthrosis of the hip joint is diagnosed.
Post-traumatic hip osteoarthritis often occurs in professional weight and light lifters, skydivers, loaders, and figure skaters.
The development of arthrosis of the hip joint after injury is due to a violation of the congruence (comparability) of the articular surfaces, a decrease in the quality of the blood supply to the joint components, and prolonged immobilization. As a result of prolonged immobility, not only impaired blood circulation occurs in the fixed area, but also shortening of the muscles, a decrease in their tone. The probability of post-traumatic arthrosis is significantly increased when an improper situation or untimely treatment is carried out, which leads to the preservation of defects of varying severity. Also, the risks of its development increase with excessively early loading of the joint and inadequate, even too intense, exercise therapy started late or vice versa early.
Sometimes the disease occurs after surgical interventions on the hip joint due to the formation of scars and additional trauma to the tissues. Although in some cases, surgery is the only way to eliminate the consequences of the injury.
Excessive loads can also lead to changes in the hip joint, as they lead to microtrauma. Regular tissue damage activates the division process of chondrocytes (cartilage tissue cells). This is accompanied by an increase in the intensity of the production of cytokines, which are normally produced in small quantities. Cytokines are mediators of inflammation, in particular, the cytokine IL-1 leads to the synthesis of specific enzymes that destroy the hyaline cartilage of the hip joint.
In addition, high loads can cause microfractures of the subchondral plate. This leads to their gradual compaction and the formation of bony growths on the surface, called osteophytes. They can have sharp edges and cause further damage to the joint, as well as injury to surrounding tissue.
The subchondral plate is the extreme part of the bone that is in direct contact with the hyaline cartilage.
In some cases, it is not possible to determine exactly what caused the development of degenerative dystrophic changes in the hyaline cartilage of the femoral head and acetabulum. In such situations, idiopathic or primary arthrosis of the hip joint is diagnosed.
Today it has been established that the tendency to develop it can be hereditary, that is, the presence of this pathology in close relatives significantly increases the chances of developing osteoarthritis of the hip joint. Presumably, it has polygenic inheritance, that is, its development depends on the presence of many genes. Each of them individually creates mild prerequisites for the development of the disease, but when combined, it becomes a matter of time, especially when leading a sedentary lifestyle and obesity, or vice versa - hard physical work.
There is a theory that osteoarthritis of the hip joints is the result of a congenital or acquired mutation of the type II procollagen gene.
There is also secondary arthrosis of the hip joint, which develops against the background of the presence of concomitant diseases and age-related changes.
Symptoms
The disease is characterized by the appearance of pain, limited mobility and contraction in the hip joint, the severity of which directly depends on the degree of neglect of pathological changes. In the final stages of development, a shortening of the affected leg and complete immobility of the hip joint can be observed, which is due to the complete fusion of the bony structures that form it.
Initially, the disease may progress without pronounced signs and cause short-term mild pain. As a rule, they appear after physical exertion, in particular, walking, carrying heavy loads, squatting, bending over. But as the degenerative-dystrophic changes in the joint progress, the pain intensifies. Over time, they not only become more intense, but also last longer, and the interval between the start of physical activity and its appearance is also reduced. At the same time, rest, even a long one, may not bring relief. Subsequently, pain can torment a person even with prolonged immobility of the hip joint, for example, after a night's sleep.

If intra-articular structures impinge on nearby nerves, pain can radiate to the groin, buttocks, thigh, and knee. However, they tend to intensify with hypothermia. At the last stage of the development of the disease, the pain becomes unbearable. This causes an unconscious desire to feel sorry for the leg and put less stress on it, which leads to lameness.
Another symptom of osteoarthritis of the hip joint is decreased range of motion. In most cases, there is a limitation in the ability to rotate the leg in and out, to lift the leg bent at the knee toward the chest. Over time, the so-called morning stiffness occurs, which disappears after the patient "diverges". Subsequently, a compensatory curvature of the pelvis is possible, which leads to a change in gait. In the future, patients completely lose the ability to perform certain movements with the affected leg.
If arthrosis of both hip joints develops at the same time, the development of the so-called waddling gait with the retracted pelvis and the body deviated forward is observed.
All this can be accompanied by the formation of edema in the hip joint. But in the presence of excess weight, they can go unnoticed.
Often during movements, especially extensors, a crunch occurs in the affected joint. It is a consequence of the exposure of the bony surfaces of the femoral head and acetabulum and their friction against each other. In this case, there is a sharp increase in pain.
Also, with arthrosis of the hip joint, painful spasms of the femoral muscles may occur. With extremely advanced degenerative-dystrophic diseases, when the joint space almost completely disappears and the femoral head begins to flatten, shortening of the affected limb by 1 cm or more is observed.
In general, there are 3 degrees of osteoarthritis of the hip joint:
- Grade 1: The joint space of the hip joint is narrowed and the edges of the bony structures are slightly pointed, indicating the beginning of the formation of osteophytes. Clinically, there is a little pronounced pain syndrome and some movement restrictions.
- Grade 2: The joint space is narrowed by more than 50% but less than 60%. Important osteophytes are observed, as well as signs of cysts in the epiphyses of the bones. Patients note significant limitations of movements in the hip joint, the presence of a crunch during movements, pain and atrophy of the thigh muscles of varying severity can be traced.
- Grade 3 - the joint space is reduced by more than 60% or is completely absent, and osteophytes occupy a large area and are large in size, subchondral cysts are observed. The hip joint is stiff, the pain can become unbearable.
Diagnosis
The appearance of pain and other symptoms characteristic of arthrosis of the hip joints is the reason for contacting an orthopedist. The doctor may suspect its presence, especially if she has suffered hip or pelvic injuries in the past, already based on the data obtained during the interview and examination.
The presence of arthrosis of the hip joint is indicated by pain, the intensity of which increases over several years. Much less often, there is a rapid development of degenerative-dystrophic changes, when several months pass from the appearance of the first signs to a powerful permanent pain syndrome. It is characterized by increased pain when standing or doing physical work. Also, for arthrosis, the presence of morning stiffness is typical, which lasts up to half an hour, and also occurs after prolonged immobility. Gradually, there is an increase in mobility restrictions and deformation of the hip joint, which in the later stages of development, the orthopedist can notice during the examination.
However, all patients are necessarily assigned instrumental methods of investigation, with the help of which it will be possible to confirm the presence of arthrosis of the hip and establish its degree, as well as differentiate it from some other diseases accompanied by similar symptoms. As a rule, diagnosis is carried out using:
- X-ray - allows you to detect the main signs of arthrosis, in particular, the narrowing of the joint space and the presence of osteophytes. But recently, CT has become a more informative research method, which makes it possible to assess the state of the hip joint more accurately.
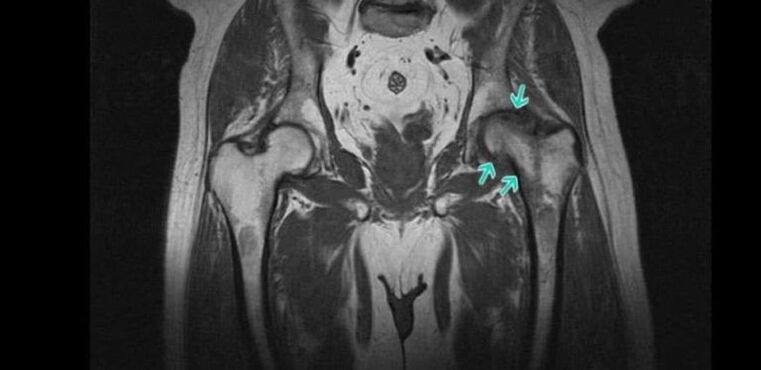
- Magnetic resonance imaging is a highly informative method of diagnosing various changes in the state of soft tissue structures, including cartilage tissue, which makes it possible to detect the slightest signs of hyaline cartilage degeneration.
Also, patients may be prescribed laboratory tests, including KLA, OAM, a biochemical blood test, etc. They must establish concomitant diseases that have created prerequisites for the development of secondary arthrosis of the hip joint.
Treatment of osteoarthritis of the hip joint without surgery
Treatment of degenerative-dystrophic changes in the hip joint through conservative therapy methods is possible only with arthrosis of the first and second degree. The prescribed measures can improve the patient's condition, stop or at least slow down the progression of the pathology and thus maintain the ability to work. But they cannot lead to a complete regression of the changes that have already occurred in the joint.
Today, as part of the conservative treatment of arthrosis of the hip joint, the following is prescribed:
- drug therapy;
- exercise therapy;
- physiotherapy.
Additionally, patients are advised to make certain lifestyle adjustments. So, in the presence of excess weight, it is worth taking measures to reduce it, that is, increasing the level of physical activity and reconsidering the nature of nutrition. If the patient is actively engaged in sports and overloads the joint, which causes microtrauma to it, it is recommended to reduce the intensity of training.
medical therapy
Drug therapy for arthrosis of the hip joint is always complex and includes drugs from different groups aimed at reducing the severity of symptoms of the disease and improving the flow of metabolic and other processes in the joint. It's:
- NSAIDs - drugs with anti-inflammatory and analgesic effects, produced both orally and in the form of local agents, which allows you to choose the most effective and convenient option for use;
- corticosteroids - drugs that have powerful anti-inflammatory properties and are used in most cases in the form of an injectable solution, since when choosing systemic therapy they provoke the development of unwanted side effects;
- chondroprotectors - drugs synthesized on the basis of natural components of cartilage tissue used by the body to restore it (prescribed for long courses);
- muscle relaxants - drugs indicated for muscle spasm, which causes pain of varying severity;
- B vitamins - help improve nerve conduction, which is required for the development of carpal tunnel syndrome;
- preparations that improve microcirculation - help to increase the intensity of blood circulation in the affected area, which leads to an increase in the rate of metabolic processes and helps restore damaged cartilage.
If concomitant diseases are detected, consultation of related specialists and appropriate treatment is indicated.
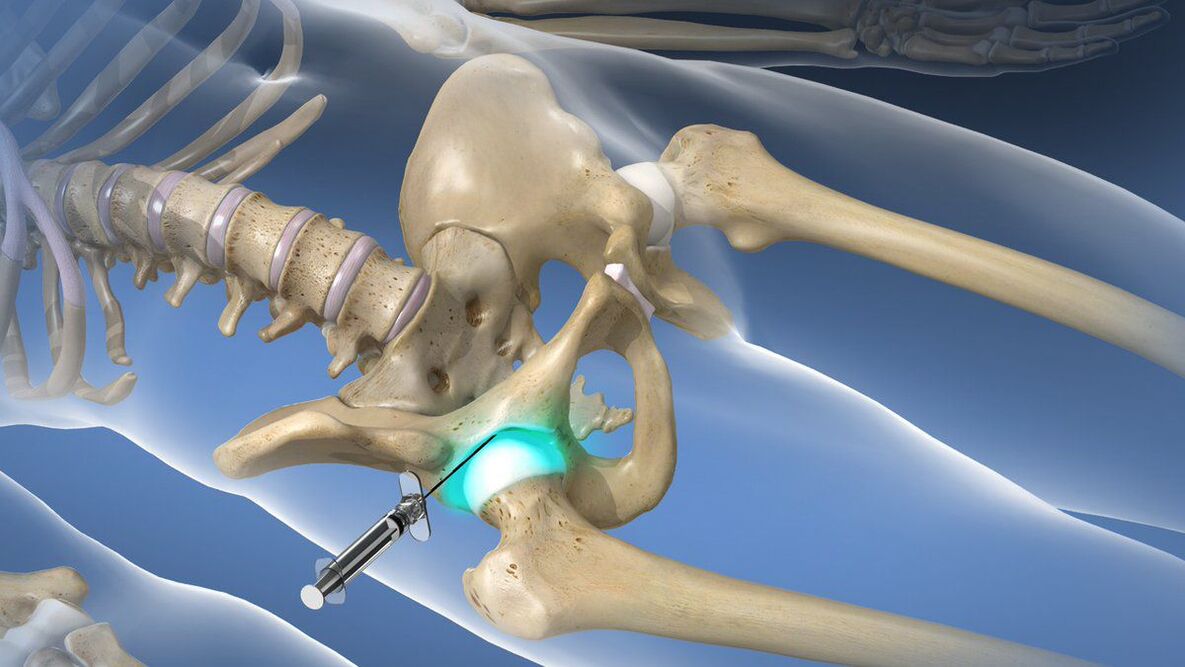
With a very strong and debilitating pain syndrome that cannot be eliminated with the help of prescribed NSAIDs, intraarticular or periarticular blocks can be performed. They involve the injection of a local anesthetic in combination with a corticosteroid directly into the joint cavity, which quickly leads to an improvement in well-being. But procedures of this type can only be performed in a medical institution by a qualified specialist, otherwise there is a high risk of complications.
exercise therapy

Physiotherapy exercises play one of the main roles in the non-surgical treatment of hip osteoarthritis, both in its idiopathic and post-traumatic forms. But a set of exercises should be selected individually, taking into account the nature of the previous injury, the level of physical development of the patient and the existing concomitant diseases.
Exercise therapy should be performed daily in comfortable conditions without rushing. All movements should be performed smoothly, without jerking, so as not to damage the already deformed hip joint. This will allow:
- reduce the intensity of the pain syndrome;
- increase joint mobility;
- reduce the risk of muscle atrophy;
- increase the intensity of blood circulation and metabolic processes.
Physiotherapy
To increase the effectiveness of the prescribed measures, patients with arthrosis of the hip joint are often recommended to undergo a course of physiotherapy procedures. Traditionally, those that have anti-inflammatory, anti-edematous and analgesic effects are chosen. It's:
- ultrasound therapy;
- electrophoresis;
- magnet therapy;
- laser therapy;
- shock wave therapy, etc.
In some cases, plasmolifting is indicated, that is, the introduction of the patient's own blood plasma, purified and saturated with platelets. To obtain it, venous blood is taken, which is then subjected to centrifugation. As a result, it is divided into erythrocyte mass and plasma, which is used to treat degenerative-dystrophic changes in the hip joint.
Surgery for osteoarthritis of the hip joint
When arthrosis of the hip joint of the third degree is diagnosed, surgical intervention is indicated for patients. It can also be carried out with the ineffectiveness of conservative therapy and persistent pain and mobility restrictions already at the second stage of the development of the disease.
In general, the indications for hip surgery are:
- a significant decrease in the size of the joint space;
- the presence of severe and persistent pain;
- significant mobility restrictions.
The most effective and safe operation for arthrosis of the hip joint is arthroplasty. Today it is recognized as the gold standard for the treatment of this pathology, regardless of the reasons for its development. The essence of this type of surgical intervention is to replace part or all of the components of the hip joint with artificially created endoprostheses. The prostheses themselves are made of biocompatible materials and are durable.
Its installation allows you to fully restore the normal mobility of the pathologically altered hip joint, eliminate pain and give the patient the opportunity to lead a full life. For each patient, the type of arthroplasty is selected individually based on the degree of destruction of various components of the joint.
The most effective is the total or total hip arthroplasty. It consists of the replacement of the entire joint with an artificial endoprosthesis, that is, the acetabulum, the femoral head and its neck. Such prostheses can serve uninterruptedly for 15-30 years and guarantee the restoration of the full volume of the functioning of the joint.
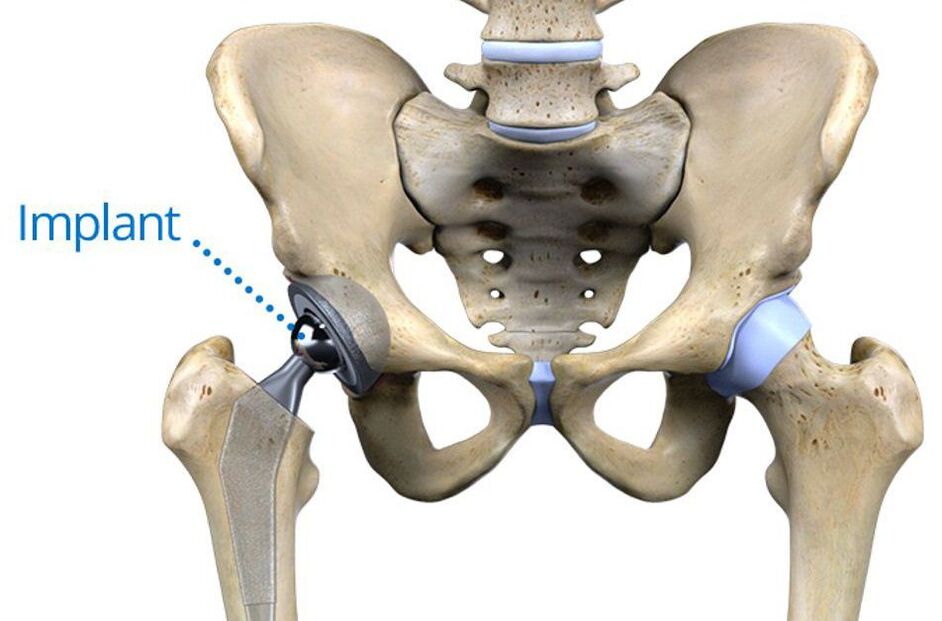
They are installed without cement or with the help of special cement. The first method is more suitable for young patients, since it consists of fixing the prosthesis in the pelvis as it grows into the spongy layer of its own bone. For older people, the method of installing an endoprosthesis with cement is more suitable, which firmly attaches the artificial material to the bone surfaces even in the presence of osteoporosis.
If the normal hyaline cartilage lining the surface of the acetabulum is preserved, patients may be offered a partial arthroplasty. Its essence is to replace only the head and neck of the femur with an endoprosthesis. Today, there are 2 types of such structures: monopolar and bipolar.
The former are less reliable, after their installation a total arthroplasty is later necessary. This is because the replaced artificial femoral head rubs directly against the cartilage of the acetabulum when making movements, causing it to wear out faster.
Bipolar endoprostheses do not have such a disadvantage, since in them the artificial femoral head is already enclosed in a special capsule, which is located next to the acetabulum. Therefore, the cartilage that covers it does not deform, since the capsule serves as a kind of shock absorber and artificial replacement of the natural hyaline cartilage of the femoral head.

However, regardless of the type of stent graft performed, postoperative rehabilitation is indicated for all patients. It consists in the appointment of drug therapy, exercise therapy and therapeutic massage. Recovery time depends on individual characteristics. But it is important to remember that the effectiveness of the operation directly depends on the quality of compliance with the doctor's recommendations during the rehabilitation period.
Thus, arthrosis of the hip joint is a common disease of the musculoskeletal system, which can occur even in the absence of direct prerequisites for its development. This pathology can lead not only to intense pain, but also to disability, so it is important to diagnose it and take measures to stop its progression even at the first signs. However, the current level of development of medicine makes it possible to cope with advanced cases of osteoarthritis of the hip joint and restore the full range of motion, as well as permanently eliminate severe pain.


















